partners :IBISC (univ Evry, université Paris-Saclay), centre hospitalier sud-francilien (CHSF)
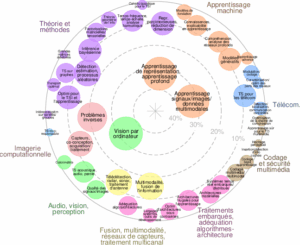
Basic AI and Data Science : apprentissage statistique en grandes dimensions
Specialized ML and AI : signal, image, vision
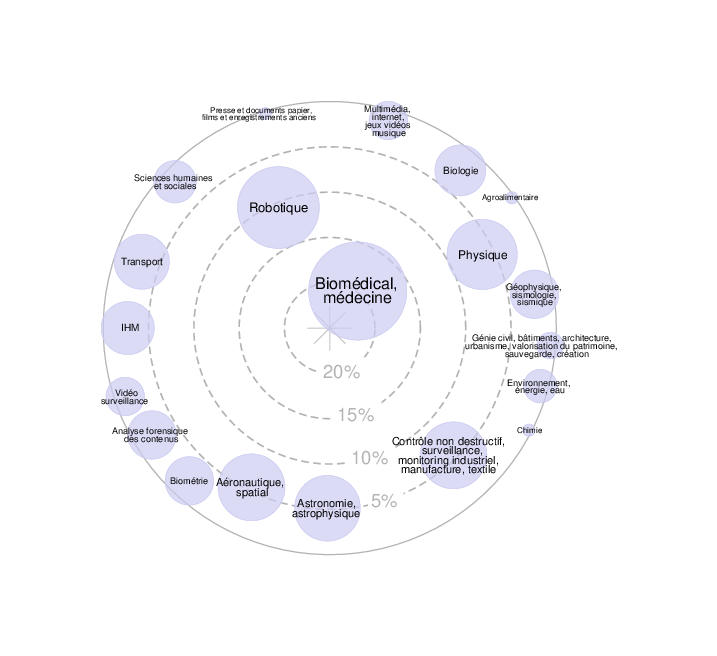
Application domain : médecine de précision, imagerie par RM
Mots-clés deep learning, imagerie multi-modale, apprentissage faiblement supervisé
Key-wordsmachine learning, deep tech, neuroimaging, precision medicine, stroke
Laboratoires partenaires impliqués : IBISC (UEVE)
Total duration of internship: 6 months (graduate) from February 2026
Working period: durée totale du stage onwards (flexible depending on candidate profile)
Subject:
Hypoperfusion in acute ischemic stroke indicates a hemodynamic disturbance visible across multiple MRI contrasts [Forkert et al., 2013]. Each modality provides complementary information: susceptibility-weighted imaging (SWAN/SWI) and phase highlight venous deoxygenation, time-of-flight (TOF) angiography captures arterial inflow and distal signal loss, diffusion-weighted imaging (DWI) shows early cytotoxic injury, and FLAIR reveals hyperintense vessels and edema [Mittal et al., 2009].
In practice, however, complete perfusion protocols are often missing or inconsistent.
Time constraints, patient motion, contrast contraindications, protocol variability, and scanner differences frequently limit acquisition.
This project builds on the observation that, even without perfusion imaging, other MRI sequences contain physiologically related cues. These can be combined to infer the hypoperfused volume [Oktay et al., 2018]. The main scientific goal is to develop a hetero-modal encoder that integrates any subset of sequences into a unified latent representation, from which a realistic hypoperfusion map can be reconstructed while preserving anatomical, physical, and inter-sequence
consistency.
Problem
Generating coherent hypoperfused maps from heterogeneous MRI inputs presents several difficulties [Liu et al., 2023]. First, the missing-modality problem arises because patients rarely undergo identical MRI protocols–each case may lack one or more key sequences, such as perfusion-weighted imaging or TOF angiography–making it difficult to learn consistent cross-modal correspondences. Second, the domain shift across scanners, vendors, and acquisition settings introduces strong variability in intensity distributions and spatial resolution, which can confound generative models trained on limited datasets. Third, anatomical and physiological consistency must be preserved: reconstructed hypoperfusion patterns should remain compatible with vascular territories, tissue diffusion constraints, and known hemodynamic principles [Copen et al., 2011]. Finally, data imbalance between normal and ischemic regions complicates loss design and evaluation metrics.
Internship Objectives
To address these issues, the proposed method will rely on a hetero-modal
encoder–decoder architecture trained within a variational or diffusion-based generative framework. The encoder will learn a shared latent space constrained by anatomical priors and mutual information regularization to align representations across modalities. The objectives are to design and implement a hetero-modal encoder–decoder trained in a variational or diffusion-based generative framework to synthesize hypoperfusion maps from routine MRI. Learn a shared latent space across modalities, constrained by anatomical priors and mutual information regularization, to align cross-sequence representations. Build robustness to missing sequences and scanner variability via modality dropout and adversarial domain adaptation. Preserve vessel detail and global perfusion coherence with multi-scale supervision during decoding.
Enforce physiological plausibility by integrating soft constraints (flow continuity, inter-hemispheric symmetry, empiric perfusion–diffusion links).
Application & Expected Impact
Quantify the ischemic ”mismatch” (penumbra) as the volume difference/ratio between perfusion deficit and diffusion core, and assess its clinical utility for reperfusion triage when onset is uncertain and for prognosticating treatment benefit. Deliverables include code, trained models, ablation studies, and validation on retrospective cohorts with reporting suited for a manuscript draft.
Candidate profile
We look for strongly motivated candidates (i) coming from a math, physics, computer science or engineering diploma (ii) having a strong mathematical background, notably in linear algebra, analysis, probability and statistics, in machine learning and deep learning (iii) having good programming skills on some scientific language, preferably python. Knowledge of medical imaging, particularly MRI, is not required, but is a strong plus. Knowledge of basic optimization theory is also appreciated.
Practical information
The intern will be mainly hosted at the UFR science and technology (40 rue du Pelvoux) close to the city center. However, he/she may also spend some periods at the Hospital of Corbeil.
The monthly internship gratification is of about 670 euros.
Application procedure: send a motivation letter, a CV and your University transcript (relevé de notes) since 1st year BSc to {vincent.vigneron,hichem.maaref}@univ-evry.fr.
What we offer
Hands-on experience with cutting-edge AI techniques for medical imaging.
Tackle real-world, high-impact healthcare problems using deep learning.
Close mentorship from experienced researchers at the IBISC laboratory.
Opportunities to co-author publications and present your work at conferences.
Continuation into PhD studies
Contact
{hichem.maaref, vincent.vigneron}@ibisc.univ-evry.fr
References
[Copen et al., 2011] Copen, W. A., Schaefer, P. W., and Wu, O. (2011). Mr perfusion imaging in acute ischemic stroke. Neuroimaging Clinics of North America, 21(2):259–283, x.
[Forkert et al., 2013] Forkert, N. D., Kaesemann, P., Treszl, A., Siemonsen, S., Cheng, B., Handels, H., Fiehler, J., and Thomalla, G. (2013). Comparison of 10 ttp and tmax estimation techniques for mr perfusion-diffusion mismatch quantification in acute stroke. American Journal of Neuroradiology, 34:1697–
1703.
[Liu et al., 2023] Liu, C.-F., Hsu, J., Xu, X., Kim, G., Sheppard, S. M., Meier, E. L., Miller, M. I., Hillis,
A. E., and Faria, A. V. (2023). Digital 3d brain mri arterial territories atlas. Scientific Data, 10(1):74.
[Mittal et al., 2009] Mittal, S., Wu, Z., Neelavalli, J., and Haacke, E. M. (2009). Susceptibility-weighted imaging: technical aspects and clinical applications. AJNR American Journal of Neuroradiology, 30(2):232–252.
[Oktay et al., 2018] Oktay, O., Schlemper, J., Folgoc, L. L., Lee, M., Heinrich, M., Misawa, K., Mori, K., McDonagh, S., Hammerla, N. Y., Kainz, B., Glocker, B., and Rueckert, D. (2018). Attention u-net: Learning where to look for the pancreas. arXiv preprint arXiv:1804.03999.